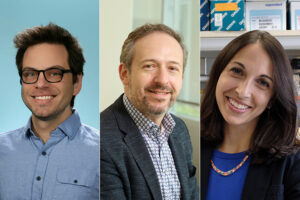
Meet some of our faculty and residents
Apply to join our faculty or staff
Providing outstanding training opportunities

Supportive culture
Our dedicated faculty and staff provide unparalleled mentorship, support and guidance to our graduates, who have incredibly high job placement rates.

In-depth experience
With such a diverse patient population and broad range of clinical expertise, our graduates are well prepared to work in any field they choose.

Groundbreaking research
From basic science to clinical studies, our trainees have access to and are encouraged to purse a broad range of research interests to provide a strong foundation.
Leading the way in diagnostic lab services
The Department of Pathology & Immunology provides consultation for clinical caregivers and supervising laboratories to ensure more accurate diagnoses that allow for the most effective treatment delivery.
State-of-the-art facilities
Our core facilities are full-service centers that provide the most advanced technology to support basic and translational research, as well as diagnostic activities at the School of Medicine and beyond. We strive to provide physicians with the best and most accurate information, while keeping turnaround times low.

Mentors who are leaders in their field

Carey-Ann Burnham, PhD
Professor of Pathology & Immunology, Molecular Microbiology, Pediatrics and Medicine

Jeffrey Gordon, MD
Dr. Robert J. Glaser Distinguished University Professor,
Professor, Pathology & Immunology

Erika Crouch, MD, PhD
Professor, Pathology & Immunology

Gautam Dantas, PhD
Conan Professor of Laboratory and Genomic Medicine, Professor, Pathology & Immunology, Biomedical Engineering, Molecular Microbiology, Pediatrics